Considering Astigmatism Correction for Vision Improvement

If you're considering astigmatism correction for vision improvement,
Q. Is it advisable to visit an ophthalmologist if I experience eye twitching?
Eye twitching, if temporary, might be due to fatigue or stress. However, frequent occurrences could indicate neurological issues or ophthalmic conditions, warranting a visit to an ophthalmologist.
Q. What benefits can I receive at an ophthalmologist's office?
You can receive basic check-ups like vision tests, intraocular pressure measurements, and fundus examinations, as well as early disease diagnosis and treatment consultations.
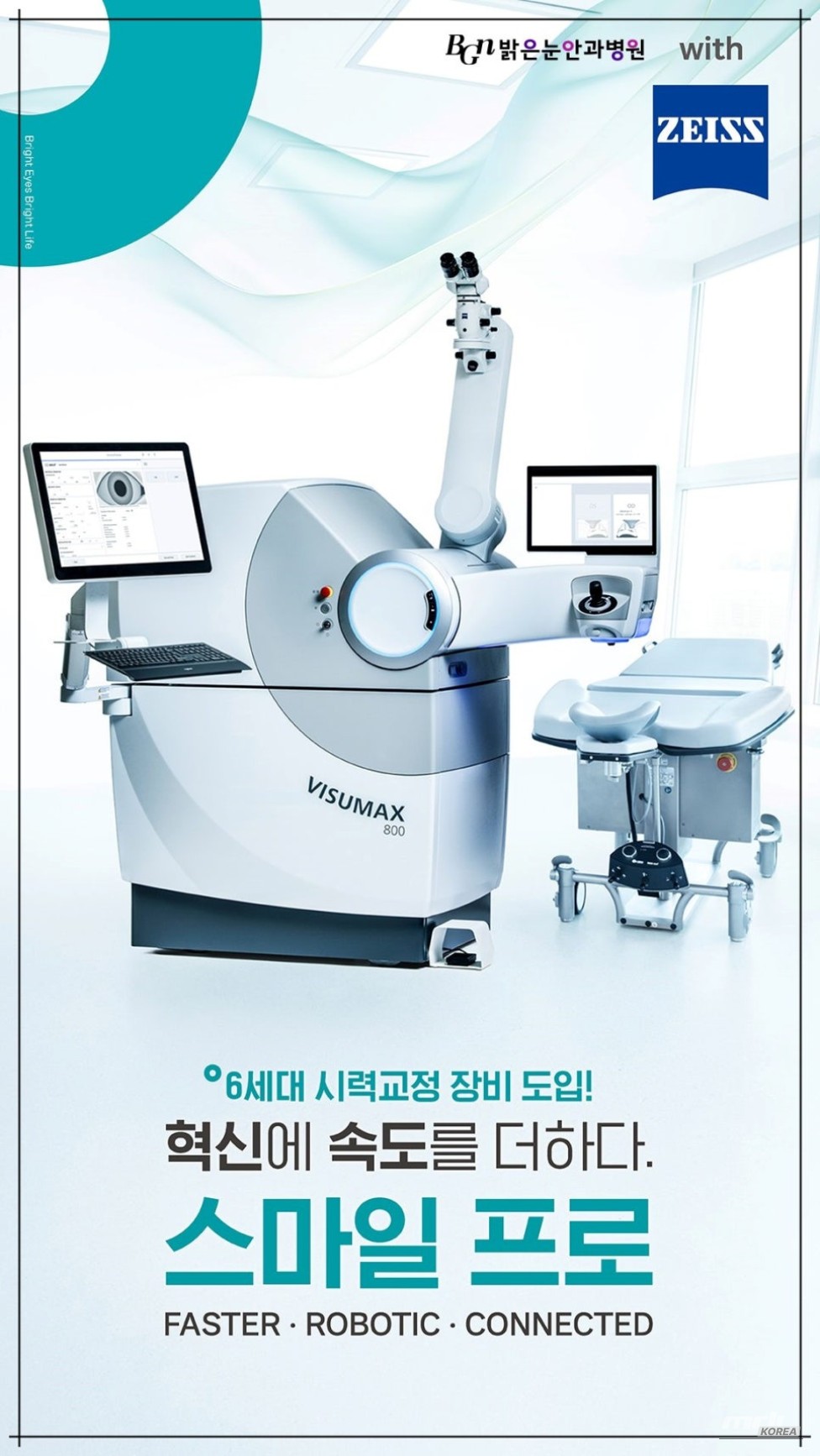
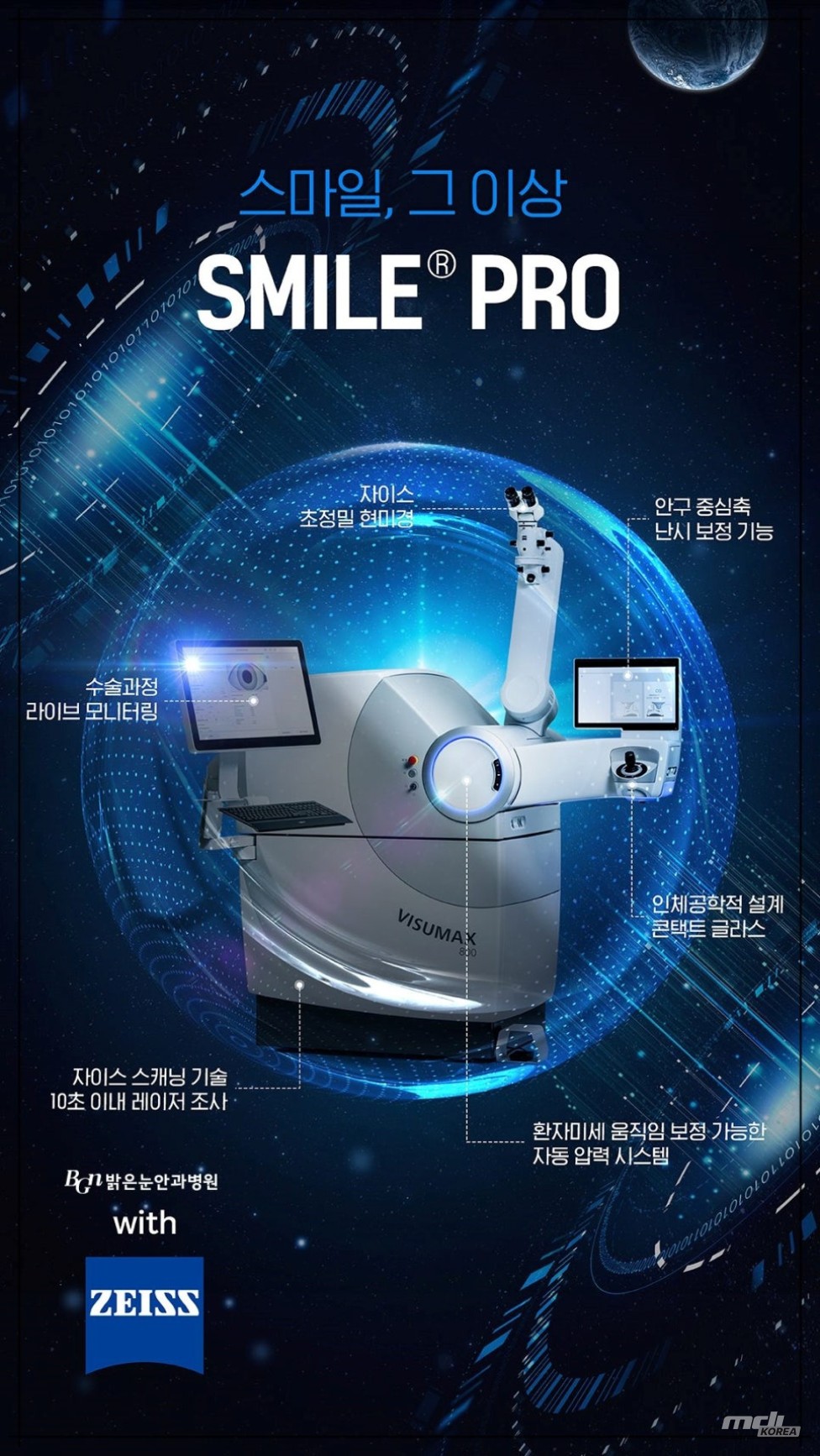
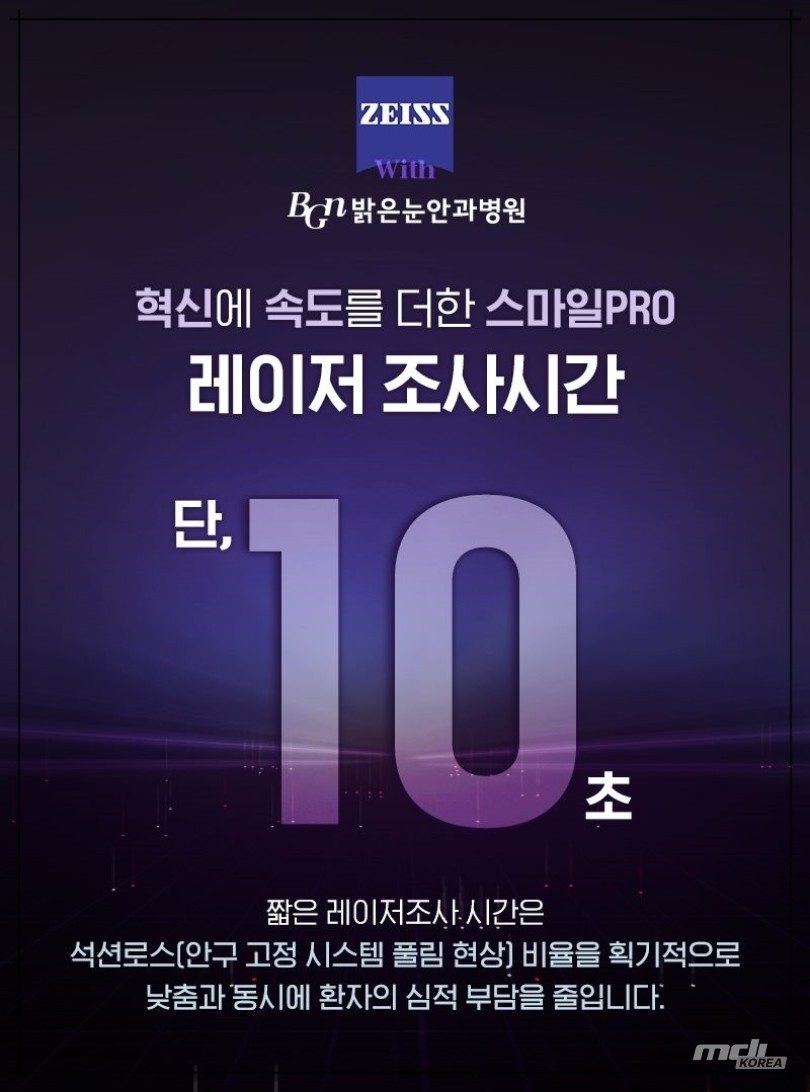
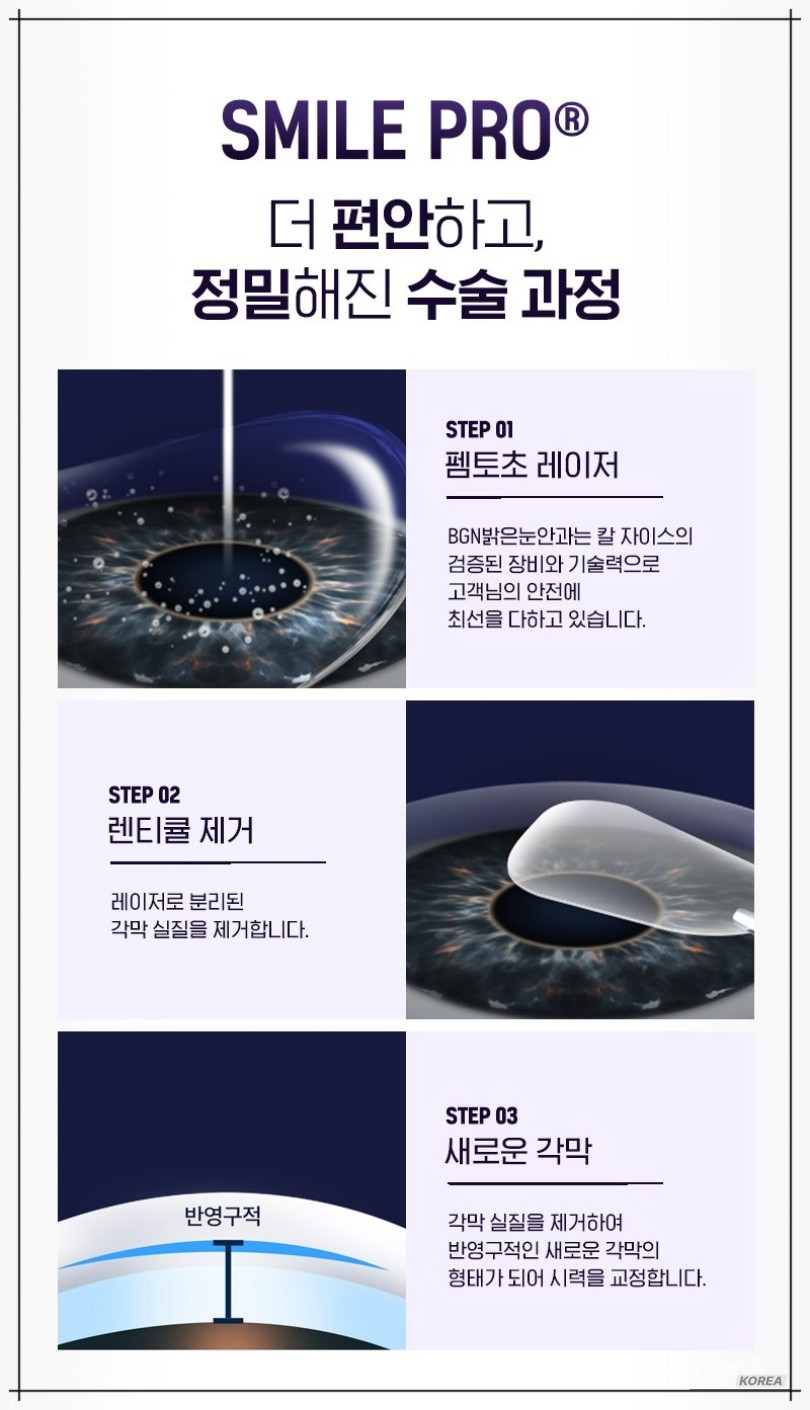
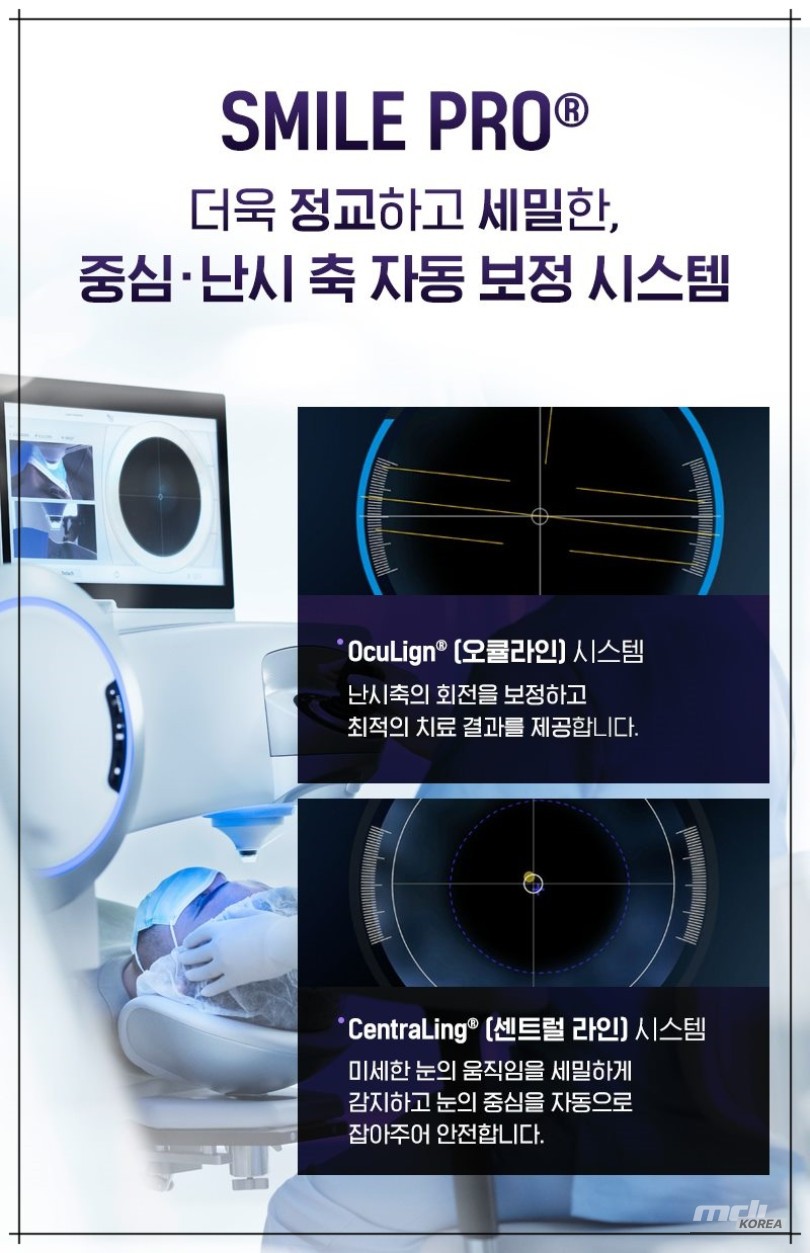
SMILE Pro is a vision correction surgery that involves creating a small tunnel in the cornea to separate and extract a thin tissue called a lenticule. A key feature is that the laser precisely separates only the necessary area without widely incising the corneal surface. It adjusts the myopia and astigmatism correction range according to the design. The core process involves detailed analysis of the corneal shape to align the center and axis, with alignment management crucial for reducing rotational errors.
If astigmatism is the main concern, the stability of the axis direction, changes in pupil position, and the tendency of ocular torsion are checked together during the initial consultation to establish a plan. The concept applied here is to reflect the astigmatic axis in the design, aiming for symmetrical refraction. Causes can include corneal curvature asymmetry, genetic predisposition, surface changes due to long-term contact lens wear, habits like eye rubbing, and corneal deformation from accidents.
At night, the pupil enlarges, increasing the influence of peripheral asymmetry, which can make light scattering or starbursting more prominent. SMILE Pro quantifies this asymmetry in the surgical design stage to determine the correction amount and axis, and eye tracking and real-time alignment verification are performed to maintain centrality. Whether to include astigmatism correction in the design is determined based on corneal thickness, area, and predicted movement.
Symptoms include not only blurriness and double vision but also a faster rate of fatigue accumulation. If focus frequently wavers in situations requiring a fixed gaze, such as computer work or driving, the eye muscles can become excessively tense, leading to headaches.
In low-light environments, light scattering increases, reducing distance readability. When proceeding with SMILE Pro, the difference in pupil size between day and night is considered to determine where to place the center and how much torsional compensation to reflect.
In this decision-making process, the design values of astigmatism correction are adjusted together to establish a balanced target vision and stability. The diagnostic process involves a step-by-step evaluation of corneal topography and thickness maps, pupil size changes, tear film stability, and eye torsion patterns. The topography visualizes differences in horizontal and vertical curvature, asymmetry distribution, and quadrant-specific slopes, providing a basis for determining which direction and how much to correct.
The thickness map is a key data point for assessing safety margin, and measurements can fluctuate in dry eyes, so consistency is ensured through repeated measurements. If the nighttime pupil is large, expanding the optical zone is considered, and if there are fine irregularities in the cornea, the option of postponing surgery or changing the method is also considered.
The goal of astigmatism correction is reflected throughout this entire procedure. The treatment method involves either SMILE Pro alone or, if necessary, adding a correction procedure for minor residual astigmatism.
The laser first creates two layers of lenticule boundary surfaces inside the cornea, then separates and extracts the tissue through a small incision. Maintaining center and axis alignment is crucial at this time, and head rotation and micro-torsion are compensated for using the immediate baseline. On the day of the visit, the procedure proceeds in the order of preparation, laser, and recovery confirmation. The surgery time is not long, but ample time is allowed for stabilization confirmation.
If the possibility of residual refractive error is anticipated, a confirmation procedure is included in the follow-up examination plan, and the need for additional astigmatism correction design is reviewed in the subsequent stage. A key point to note is to set expectations realistically.
If the pupil is large or the corneal thickness margin is small, there may be limitations in the design. If the corneal surface is dry, initial blurring or foreign body sensation may be prolonged, so tear film stabilization is checked first during the examination stage. Adhering to the prescribed eye drop and protection guidelines before surgery can reduce fluctuations in the recovery process.
For a few days after surgery, light scattering may be felt, but it usually tends to subside over time. If necessary, additional tests should be performed to recheck residual refractive error and axis alignment. Continuing follow-up observations according to the provided schedule can help achieve results that align with the design goals. Before surgery, dryness indicators and corneal nerve sensitivity are assessed together.
If dryness indicators are unstable, initial blurring may be prolonged, so the timing should be adjusted or an eye drop plan should be established first. If ocular torsion is large, the axis alignment is compensated for by re-aligning the baseline in the lying position. On the day of surgery, it is good to practice opening the eyes without squeezing them excessively. During the laser stage, focus the gaze on the marked point and check for residual tissue in the tunnel area after completion.
This process is conducted under the guided procedures and safety rules, and unreasonable schedule compression is avoided. In the recovery stage, the speed at which the field of vision clears varies from person to person. Most people can resume daily activities the next day, but prolonged driving and monitor work should be increased slowly.
Initially, there may be light scattering and dryness, so use eye drops regularly and check the corneal surface and central alignment according to the schedule. Do not rush to evaluate residual refractive error until corneal curvature stabilizes, and confirm with repeated measurements at the scheduled time. Consider whether to make fine corrections if necessary, but prioritize the balance of corneal thickness and optical zone.
From a long-term perspective, occupation and lifestyle patterns are reflected. If night work is frequent, more weight is given to maintaining the optical zone and centrality, and if near work is frequent, the goal is set considering the burden of accommodation. It is safer to avoid habits such as rubbing the eyes strongly, which puts a burden on the corneal surface, and in dry environments, help stabilize the tear film by managing humidity and increasing rest intervals.
The strengths of astigmatism correction were revealed when the initial goals were clear and alignment and axis were repeatedly checked. The better the connection between examination, planning, procedure, and follow-up, the more stably daily clarity can be maintained.



Source :https://blog.naver.com/koikoro/224042136512
No comments yet.

